I’m writing this primarily for the benefit of other veterinarians (much like my 304/404 extraction post) because when I got started in the process and researched treatment options for discospondylitis, the information available was scant and the recommendations were quite variable. Clearly, though, there are many pet owners that perform their own research in a quest for information when their pets are showing abnormal symptoms. Hopefully both parties will find this post useful.
|
In the fall of 2007, my best dog, Bridget (4.5 year old, F(s) Boxer, 65#, 3/5 BCS)
* began losing weight (dropped to 55# over several weeks due to significant loss of muscle mass around her back)
* become significantly less active
* and moved very, very stiffly when she did get up to do something.
As August became September, she was reluctant to use stairs, she refused to play, and she was moving painfully. She was not responsive to non-steroidal anti-inflammatory therapy. And because she was a Boxer, I was thinking the worst: there must be an ugly cancer somewhere. Dwelling on the unknown is never productive, though, and pursuing answers was necessary.
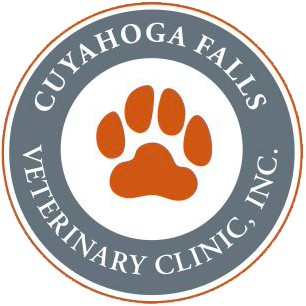
The following radiographs and commentary show her progression from mystery to diagnosis to cure of discospondylitis.
Radiograph 9/21/07
Yellow Arrow: Discospondylosis, the bony bridging from one vertebra to another, is not an abnormal finding, particularly in Boxers. While it can be a source of pain for some dogs, this degree of discospondylosis did not explain the severity of Bridget’s symptoms. Discospondylosis is very different from discospondylitis, an infection of the vertebral endplates and the intense, painful inflammation that comes with it.
Orange Arrow: This is the area that proved to be the problem point. Notice how the space is slightly more narrow than the adjacent spaces, but this narrowing in and of itself didn’t explain the severity of her symptoms.
The narrowing, combined with her symptoms suggested discospondylitis. I make particular use of the word “suggested” because radiographic evidence of discospondylitis lags behind the histologic (tissue) and anatomic changes at the vertebral level. Also, I had never seen a case of this before, nor had my DVM wife, nor had my DVM father. This is not a common disease at all. It was not until much later that the severity of the disease could be appreciated radiographically, as seen in later films below.
|
Further, there has been talk in veterinary circles about obtaining urine cultures or blood cultures to aid in the diagnosis of discospondylitis. I didn’t perform a urine culture with Bridget. Her blood culture was negative. These tests may be helpful… or they may not be helpful.
With the help of Rod Ferguson, DVM, DACVS, at the Akron Veterinary Referral Center, antibiotic therapy was initiated based on her symptoms. As a specialist, he had seen a number of discospondylitis cases. Bridget began Cephalexin 750mg every 8 hours and Baytril 136mg every 12 hours. The plan was to continue antibiotics for three months. (You read that correctly.) Pain medication was used daily at the onset (cortisone was the only treatment that gave her any relief before her diagnosis), but as the antibiotics began taking hold against her infection, we were able to wean her off of Rimadyl and Tramadol.
Radiograph 1/22/08
Orange Arrow: The vertebral endplates are no longer smooth as are the other vertebral spaces. The bone is being destroyed.
Green Arrow: Arthritic, bony changes are taking place in response to the instability of the vertebral space.
Radiograph 4/1/08
Yellow Arrow: Discospondylosis has completely bridged across the endplates of the affected area of discospondylitis. This is providing stability at the joint.
Orange Arrow: What was once an area of two lytic endplates is resolving radiographically.
Radiograph 3/13/09
Orange Arrow: The two affected vertebra have fused. Bridget always had a different arch to her back after she healed, but she was comfortable and functional.
Treatment of Discospondylitis
I’d like to refer back to the treatment plan that we used with Bridget. While Cephalexin is relatively inexpensive, Baytril is not. If we hadn’t used Baytril, we would have had to use another big-gun antibiotic (Clavamox, for instance), and these types of treatments are not inexpensive.
It should be stated very clearly that effectively diagnosing and treating discospondylitis takes time. Further, between a series of radiographs, necessary pain medication, and appropriate antibiotics, there is a significant degree of cost associated with the treatment of discospondylitis. Bridget’s story, though, demonstrates that the time, cost and effort is definitely worth it. She was back to her normal self when she was given a chance with appropriate diagnosis and therapy! When Bridget’s time with me was through, it had nothing to do with her discospondylitis.
If the information above has prompted any questions, whether you’ve got a dog that is showing signs of pain but you can’t figure out what is the cause or if you’re a veterinarian researching discospondylitis, feel free to give us a call at 330-929-3223.

Joanne Jackson, Houston
Thank you so much for your article. I have a male 2yr old Boxer named Hondo that I’m trying desperately to find a diagnosis for and Bridget’s story resonates.
Hondo has been slowing down over the last 2 months, doesn’t want to jump in or out of the SUV, doesn’t want to go up or down stairs, walking stiffly with difficulty getting up and within the last 2 weeks has deteriorated to barely able to walk. I’ve been to 2 different vets, the first only offering referral for MRI under the assumption that because he’s a Boxer it was probably Degenerative Myelopathy (DM) or Intereterbral Disc Disease (IVDD). That was terrifying and if it was DM i couldn’t see putting him through an MRI if there wouldn’t be a treatment plan after diagnosis.
After researching DM & IVDD more, some of the symptoms fit but a lot of them didn’t with a major difference being that he’s only 2 and beyond the walking issue he looks to be in perfect health – shiny coat, no noticable wasting, no incontinence, good heart, he’s lost 5-8 pounds but he needed to lose a couple of lbs, nothing extraordinary on his blood work, low normal thyroid (.9), no extreme pain to touch him, although he’s now crying while laying down and can’t seem to get comfortable, but he’ll still wag his tail when he feels like it.
On 8/10/12 we went to another vet that practices western & eastern verterinary medicine and with his first chiropractic session she adjusted his mis-rotated pelvis and he pepped up for the entire day, was quiet for the wknd peppy that Monday and by Monday afternoon began a steady decline making his gait even worse than before the chiropractic session.
That Friday, 8/17/12, i took him back for another adjustment thinking his pelvis must be out of place again which was making him so stiff but his back and pelvis didn’t need adjustment and she ws concerned about how stiff he was all over making her think it might be something infectious making all of his muscles stiff. She decided to do accupuncture on him this time and if he was feeling better by Monday (8/20) she wanted me to take him to a specialist for internal diagnostics – thinking that possibly it was a tick borne infection causing his lameness. 30 minutes after treatment Hondo could barely walk – only taking small 4″ steps with his front & rear legs, panting heavily and unwilling to try to lay down unless he absolutely had to.
After informing my vet she referred me as an emergency to our diagnostic specialist clinic. 6 hrs later, more blood work, orthopedic surgeon consult, review of his pelvic X-rays taken in May 2012 (he hit a wall while chasing a squirrel, original vet diagnosed soft tissue damage to his right knee only) all the specialist could tell me was that they couldn’t determine what was causing his gait abnormalities but they would like to do muscle & nerve biopsies, on the assumption it was DM and/or they’d like to do an MRI but they weren’t sure what an MRI would show, if anything.
So we left without answers or any type of treatment to help him feel better or walk. And through a lot of tears this wknd I’ve been searching for online videos of dogs with DM or slipped discs and the things that I kept coming back to are age of onset and/or presentation of symptoms and Hondo’s symptoms are slightly similar but different at the basis of the diagnosis. Finally, I found a video of another boxer that had become paralysed because of a ‘spine infection’ but who was slowly regaining some functions.
I started searching for those key words as a cause of lameness and found discospondylitis, your article and many others that detail Hondo’s exact symptoms (even a couple of videos that are very similar to how Hondo is now walking). But the main link that i hope my vet can use to confirm a diagnosis is that Hondo’s decline has been happening since about the same time as he contracted Bordetella on 6/20/12. He completed 2 weeks of antibiotic treatment for that but he never made it back to 100% and then began the steady decline to where we are now. So we’re going to the vet tomorrow to request spinal X-rays and treatment specific to discospondylitis, and your article is definitely my main point of reference since none of the DVM’s we’ve seen to date have even referenced anything similar.
Would you be able to approximate the stages of the infection as far as time lapse and expectation of being able to regain full functionality? (If I’m on the cusp of Hondo permanently losing some functionality due to the amount of time lapsed while trying to figure out a diagnosis, I’d want to make sure he’s getting the most aggressive antibiotic treatment no matter the cost.)
Thank you again for your article, for reading my book of a ‘comment’, and for any additional information you might be able to provide. 🙂
Joanne & Hondo Lane
(This comment’s formatting has been edited to provide for easier reading. The spirit and the content has not been changed. –Dr. Ryan Gates)